Family Resources in Resources in Utah
- Utah Department of Health and Human Services Office of Substance Use and Mental Health (sumh.utah.gov) Resources and contacts
- Utah 211 (211utah.org) Search, call, text, chat, or email to find resources
- NAMI Utah (namiut.org) Support groups, training, information
- Utah Disability Law Center (disabilitylawcenter.org) Protection and advocacy for individuals with disabilities
- 211 Salt Lake County Homeless Resource List (211utah.org) Shelters, meals, counseling, and more
- Utah Department of Corrections Offender Search (corrections.utah.gov) Search for someone in prison by name or offender number
- Utah State Bar (utahbar.org) Legal assistance
How many people in Utah have SMI?
individuals with severe mental illness.
individuals with SMI who receive treatment in a given year.
of the adult population is estimated living with a SMI in the United States.
State psychiatric hospital beds in Utah
2023 total beds: 246
- Civil beds: 120
- Forensic beds: 126
2023 beds per 100,000 people: 7.3
Click here for more information about state psychiatric hospital beds in Utah.
A minimum of 50 beds per 100,000 people is considered necessary to provide minimally adequate treatment for individuals with severe mental illness. Utah fails to meet this minimum standard.
For Additional Information
Data is a powerful tool to advocate for change. Curious about a specific data point in your state? Reach out to us at ORPA@treatmentadvocacycenter.org
Fast Facts on SMI in Utah
Deinstitutionalization, outdated treatment laws, discriminatory Medicaid funding practices, and the prolonged failure by states to fund their mental health systems drive those in need of care into the criminal justice and corrections systems.
21%
2,803
246
11 to 1
2021 Utah State Mental Health Agency's expenditures
Every state receives block grant funding from the federal government to provide mental health services to their community. Below is some information about how these dollars are spent and compares to other state spending.
$268,235,228
28%
$4,667
1.4%
Utah's Treatment Laws
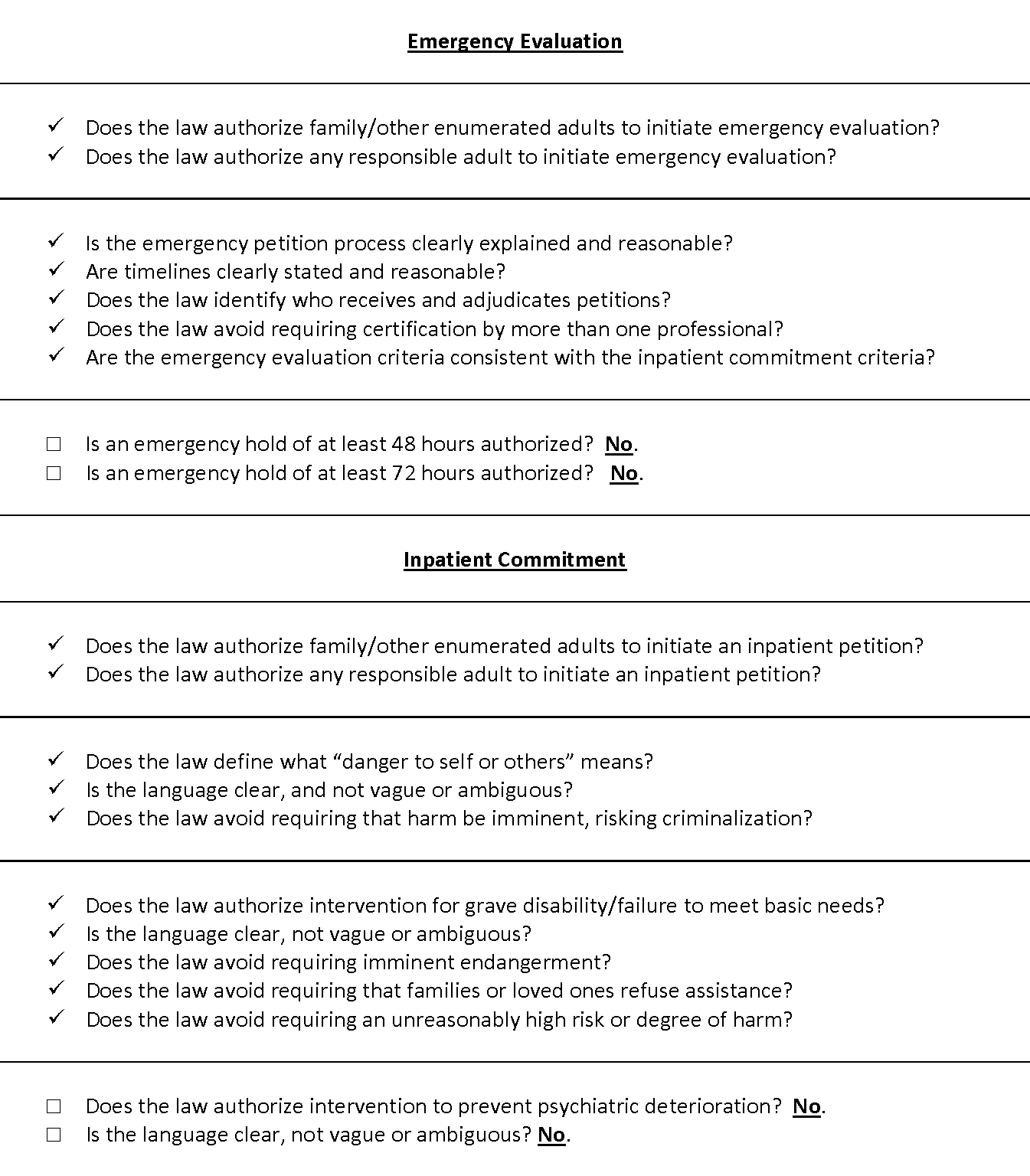
UTAH CODE ANN. § 26B-5-332 (1) A responsible individual who has credible knowledge of an adult’s mental illness and the condition or circumstances that have led to the adult’s need to be involuntarily committed may initiate an involuntary commitment court proceeding by filing, in the court in the county where the proposed patient resides or is found, a written application that includes: (a) unless the court finds that the information is not reasonably available, the proposed patient’s: (i) name; (ii) date of birth; and (iii) social security number; (b) (i) a certificate of a licensed physician or a designated examiner stating that within the seven-day period immediately preceding the certification, the physician or designated examiner examined the proposed patient and is of the opinion that the proposed patient has a mental illness and should be involuntarily committed; or (ii) a written statement by the applicant that: (A) the proposed patient has been requested to, but has refused to, submit to an examination of mental condition by a licensed physician or designated examiner; (B) is sworn to under oath; and (C) states the facts upon which the application is based; and (c) a statement whether the proposed patient has previously been under an assisted outpatient treatment order, if known by the applicant. UTAH CODE ANN. § 26B-5-331. (1) An adult shall be temporarily, involuntarily committed to a local mental health authority upon: (a) a written application that: (i) is completed by a responsible individual who has reason to know, stating a belief that the adult, due to mental illness, is likely to pose substantial danger to self or others if not restrained and stating the personal knowledge of the adult’s condition or circumstances that lead to the individual’s belief; and (ii) includes a certification by a licensed physician, licensed physician assistant, licensed nurse practitioner, or designated examiner stating that the physician, physician assistant, nurse practitioner, or designated examiner has examined the adult within a three-day period immediately preceding the certification, and that the physician, physician assistant, nurse practitioner, or designated examiner is of the opinion that, due to mental illness, the adult poses a substantial danger to self or others; or (b) a peace officer or a mental health officer: (i) observing an adult’s conduct that gives the peace officer or mental health officer probable cause to believe that: (A) the adult has a mental illness; and (B) because of the adult’s mental illness and conduct, the adult poses a substantial danger to self or others; and (ii) completing a temporary commitment application that: (A) is on a form prescribed by the division; (B) states the peace officer’s or mental health officer’s belief that the adult poses a substantial danger to self or others; (C) states the specific nature of the danger; (D) provides a summary of the observations upon which the statement of danger is based; and (E) provides a statement of the facts that called the adult to the peace officer’s or mental health officer’s attention. (2) If at any time a patient committed under this section no longer meets the commitment criteria described in Subsection (1), the local mental health authority or the local mental health authority’s designee shall document the change and release the patient. (3) (a) A patient committed under this section may be held for a maximum of 24 hours after commitment, excluding Saturdays, Sundays, and legal holidays, unless: (i) as described in Section 26B-5-332, an application for involuntary commitment is commenced, which may be accompanied by an order of detention described in Subsection 26B-5-332(4); (ii) the patient makes a voluntary application for admission; or (iii) before expiration of the 24 hour period, a licensed physician, licensed physician assistant, licensed nurse practitioner, or designated examiner examines the patient and certifies in writing that: (A) the patient, due to mental illness, poses a substantial danger to self or others; (B) additional time is necessary for evaluation and treatment of the patient’s mental illness; and (C) there is no appropriate less-restrictive alternative to commitment to evaluate and treat the patient’s mental illness. (b) A patient described in Subsection (3)(a)(iii) may be held for a maximum of 48 hours after the 24 hour period described in Subsection (3)(a) expires, excluding Saturdays, Sundays, and legal holidays. (c) Subsection (3)(a)(iii) applies to an adult patient. (4) Upon a written application described in Subsection (1)(a) or the observation and belief described in Subsection (1)(b)(i), the adult shall be: (a) taken into a peace officer’s protective custody, by reasonable means, if necessary for public safety; and (b) transported for temporary commitment to a facility designated by the local mental health authority, by means of: (i) an ambulance, if the adult meets any of the criteria described in Section 26B-4-119; (ii) an ambulance, if a peace officer is not necessary for public safety, and transportation arrangements are made by a physician, physician assistant, nurse practitioner, designated examiner, or mental health officer; (iii) the city, town, or municipal law enforcement authority with jurisdiction over the location where the adult is present, if the adult is not transported by ambulance; (iv) the county sheriff, if the designated facility is outside of the jurisdiction of the law enforcement authority described in Subsection (4)(b)(iii) and the adult is not transported by ambulance; or (v) nonemergency secured behavioral health transport as that term is defined in Section 26B-4-101. (…)
UTAH CODE ANN. § 62A-15-631(16). The court shall order commitment of an individual who is 18 years of age or older to a local mental health authority if, upon completion of the hearing and consideration of the information presented …, the court finds by clear and convincing evidence that: (a) the proposed patient has a mental illness; (b) because of the proposed patient's mental illness the proposed patient poses a substantial danger … to self or others; (c) the proposed patient lacks the ability to engage in a rational decision-making process regarding the acceptance of mental treatment as demonstrated by evidence of inability to weigh the possible risks of accepting or rejecting treatment; (d) there is no appropriate less-restrictive alternative to a court order of commitment; and (e) the local mental health authority can provide the individual with treatment that is adequate and appropriate to the individual’s conditions and needs. In the absence of the required findings of the court after the hearing, the court shall forthwith dismiss the proceedings. UTAH CODE ANN. § 26B-5-301(24). “Substantial danger” means that due to mental illness, an individual is at serious risk of: a. suicide; b. serious bodily self-injury; c. serious bodily injury because the individual is incapable of providing the basic necessities of life, including food, clothing, or shelter; d. causing or attempting to cause serious bodily injury to another individual; e. engaging in harmful sexual conduct; or f. if not treated, suffering severe and abnormal mental, emotional, or physical distress that: (i) is associated with significant impairment of judgment, reason, or behavior; and (ii) causes a substantial deterioration of the individual’s previous ability to function independently. UTAH CODE ANN. § 26B-5-301(22). “Serious bodily injury” means bodily injury that involves a substantial risk of death, unconsciousness, extreme physical pain, protracted and obvious disfigurement, or protracted loss or impairment of the function of a bodily member, organ, or mental faculty.
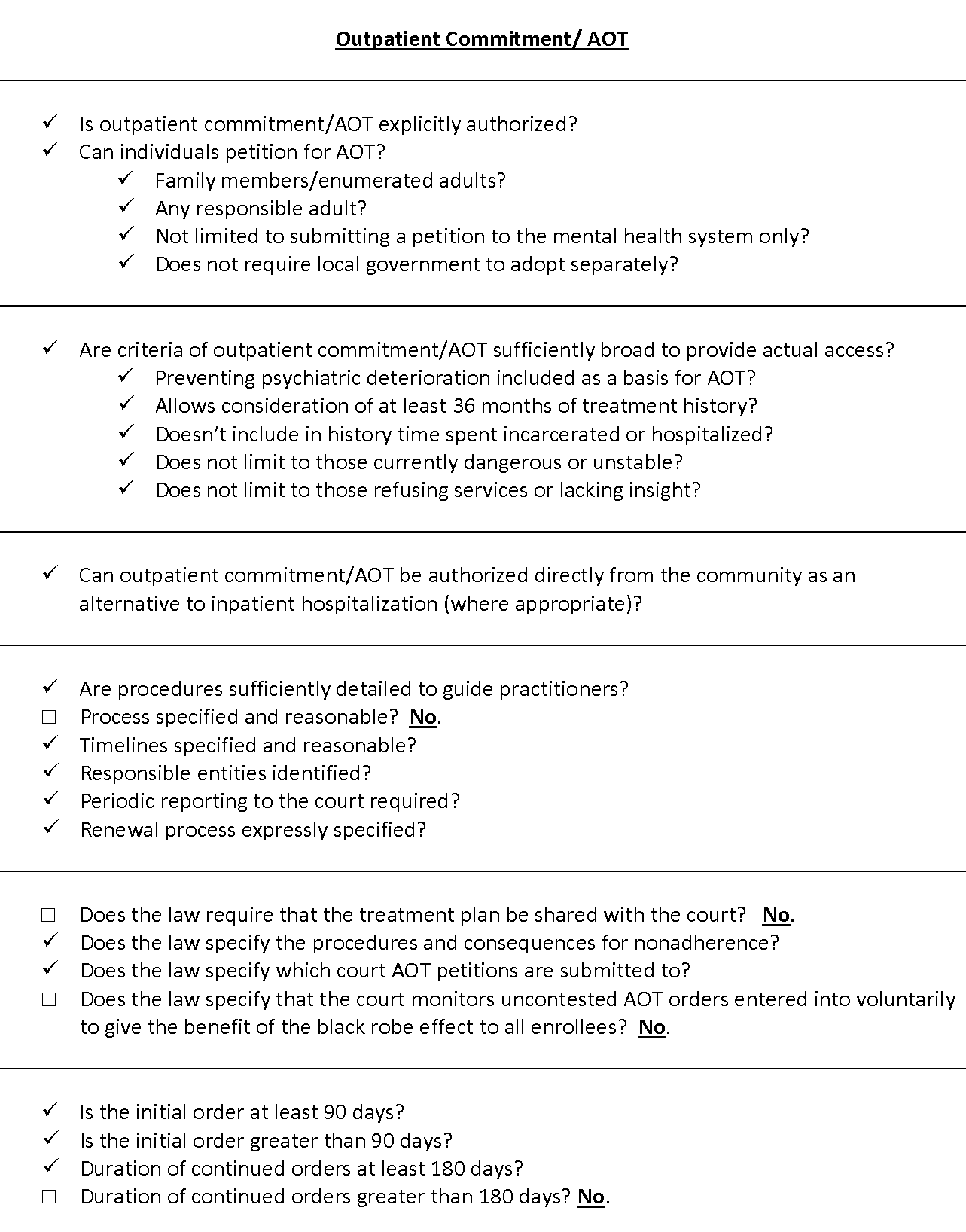
UTAH CODE ANN. § 26B-5-351 (1). A responsible individual who has credible knowledge of an adult’s mental illness and the condition or circumstances that have led to the adult’s need for assisted outpatient treatment may file, in the court in the county where the proposed patient resides or is found, a written application that includes: (a) unless the court finds that the information is not reasonably available, the proposed patient’s: (i) name; (ii) date of birth; and (iii) social security number; and (b) (i) a certificate of a licensed physician or a designated examiner stating that within the seven-day period immediately preceding the certification, the physician or designated examiner examined the proposed patient and is of the opinion that the proposed patient has a mental illness and should be involuntarily committed; or (iii) a written statement by the applicant that: (A) the proposed patient has been requested to, but has refused to, submit to an examination of mental condition by a licensed physician or designated examiner; (B) is sworn to under oath; and (C) states the facts upon which the application is based. (…) 14. The court shall order a proposed patient to assisted outpatient treatment if, upon completion of the hearing and consideration of the information presented, the court finds by clear and convincing evidence that: (a) the proposed patient has a mental illness; (b) there is no appropriate less-restrictive alternative to a court order for assisted outpatient treatment; and (c) (i) the proposed patient lacks the ability to engage in a rational decision-making process regarding the acceptance of mental health treatment, as demonstrated by evidence of inability to weigh the possible risks of accepting or rejecting treatment; or (ii) the proposed patient needs assisted outpatient treatment in order to prevent relapse or deterioration that is likely to result in the proposed patient posing a substantial danger to self or others.
Recommended updates to treatment laws
- 1
Amend Utah Code § 26B-5-331(3)(a) to extend duration of emergency hold period to a minimum of 72 hours
- 2
Add psychiatric deterioration criteria or amend grave disability criteria to include it
- 3
Amend Utah Code § 26B-5-331 in order to address procedural barriers to AOT, include a requirement that a written treatment plan be submitted to the court, and specify procedures and consequences for nonadherence
- 4
Amend Utah Code § 26B-5-331 to extend duration of continued order beyond 180 days
- 5
Adopt express procedures for the court to monitor uncontested AOT orders entered into voluntarily to give the benefit of the black robe effect to all enrollees
